Understanding the Impact of Radiation Therapy on Post-Treatment Recovery
Radiation therapy, while often crucial for cancer treatment, can have various effects on the body. This includes potential changes in the oral cavity and swallowing mechanics. The nuances of recovery, particularly the implications for proper oral function, are a significant consideration for patients undergoing radiation treatments.
Following radiation therapy, the tissues in the mouth, throat, and esophagus can experience inflammation, dryness, and impaired healing. These complications can impact a patient's ability to eat, drink, and speak. This can range from temporary discomfort to more long-lasting difficulties, demanding careful attention and management. Strategies to mitigate these challenges, such as specific dietary modifications and supportive therapies, are vital for optimal post-treatment well-being. The focus in post-treatment care is thus crucial in restoring oral health and ensuring quality of life.
Importance and Benefits of Post-Radiation Oral Care and Support
A holistic approach to oral health and nutrition after radiation therapy is essential. This includes meticulous oral hygiene practices, regular follow-up with dental professionals, and appropriate dietary adjustments to support healing and promote nutrition. Implementing preventive and supportive measures can demonstrably reduce complications and improve recovery timelines. Furthermore, these approaches contribute to maintaining or restoring patients' quality of life by preventing or addressing discomfort and allowing for improved nutritional intake.
Note: This general overview of post-radiation oral health does not provide specific medical advice. Individual cases and treatment plans vary. Patients should consult with their healthcare providers for personalized guidance and recommendations.
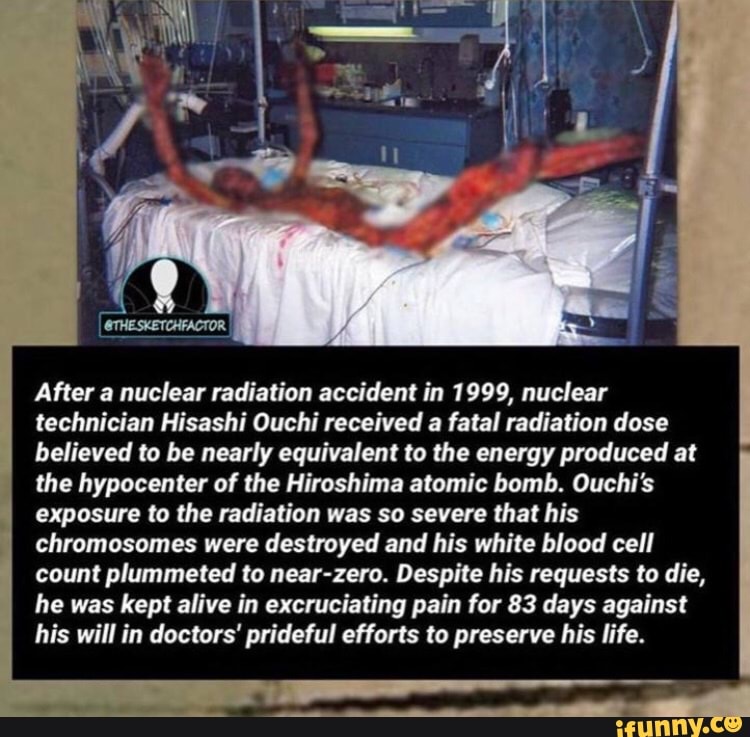
Hisashi Ouchi After Radiation
Post-radiation recovery, encompassing physical and functional aspects, is crucial for optimal patient well-being. Understanding the nuances of this process is essential for effective care.
- Oral health
- Nutritional support
- Communication
- Pain management
- Fatigue reduction
- Quality of life
- Psychological impact
These key aspects intertwine to significantly affect an individual's life after radiation treatment. For example, compromised oral health can impede nutritional intake, leading to further complications and impacting overall recovery. Effective pain management strategies are vital to enabling participation in rehabilitation exercises, thus bolstering physical function. Maintaining communication skills is equally critical for emotional well-being and social interactions. The cumulative impact of these interwoven aspects dictates the trajectory of a patient's post-treatment life. Improved quality of life after radiation is directly associated with appropriate care addressing each element. A well-rounded approach to these areas promotes successful rehabilitation and a more positive outlook on recovery.
1. Oral Health
Oral health assumes critical importance in the context of post-radiation recovery. Impaired oral function, a frequent consequence of radiation therapy, can significantly impact nutritional intake, communication, and overall quality of life. Maintaining or restoring oral health is thus a cornerstone of successful rehabilitation.
- Nutritional Implications
Radiation therapy can induce mucositis, inflammation of the oral mucosa, and xerostomia, reduced saliva production. These conditions make eating and swallowing challenging, leading to decreased food intake and potential nutritional deficiencies. Proper oral hygiene, including regular mouthwashes and soft-bristled toothbrushes, and dietary modifications (e.g., soft, bland foods) are crucial to mitigate these challenges. Adequate nutrition is essential for tissue repair and overall recovery.
- Communication Difficulties
Oral cavity and throat tissues are susceptible to damage from radiation. This damage can impair speech articulation and swallowing, creating communication challenges. Maintaining adequate oral hydration and using appropriate mouthwashes can help to minimize the impact of these difficulties. Speech therapy might also be necessary to help restore normal speech function.
- Pain Management and Discomfort
Oral discomfort and pain are common during and after radiation therapy. Oral hygiene practices can help ease discomfort. The use of topical pain relievers, as well as the guidance of a dentist or oral healthcare specialist, may also be necessary to effectively manage pain and promote comfort. Addressing pain promptly and effectively helps to improve patients' quality of life and encourages compliance with necessary treatments and dietary regimens.
- Impact on Overall Well-being
Compromised oral health significantly impacts a patient's well-being beyond immediate physical symptoms. Oral discomfort and impaired function can contribute to emotional distress, social isolation, and decreased participation in activities. Early intervention and appropriate management of oral complications are critical to maintaining an individual's overall quality of life.
In conclusion, maintaining or restoring optimal oral health is integral to a successful recovery trajectory after radiation therapy. Carefully managing potential oral complications will promote improved nutrition, reduced pain, better communication, and ultimately, a better quality of life for individuals undergoing this treatment.
2. Nutritional Support
Nutritional support is paramount in the recovery process following radiation therapy, particularly in the context of post-treatment oral health. The impact of radiation on the oral cavity often necessitates modifications to the diet, impacting nutrient intake. Malnutrition can exacerbate existing health conditions and slow recovery. Consequently, meticulously planned nutritional support is not merely advisable but essential for successful rehabilitation after radiation.
Dietary changes following radiation therapy are frequently necessary due to complications such as mucositis (inflammation of the oral mucosa), xerostomia (dry mouth), and dysphagia (difficulty swallowing). These conditions significantly restrict the types and textures of foods that can be consumed. A personalized nutritional plan must account for these limitations. For example, soft, easily digestible foods like pureed soups, yogurt, or mashed fruits might be recommended to minimize discomfort while ensuring adequate calorie and nutrient intake. Careful attention to hydration is also critical, as dry mouth can lead to dehydration, impacting overall health and well-being. Regular monitoring of nutritional status and adjustments to the diet, as per the recommendations of healthcare professionals, are critical components of successful post-radiation recovery.
The importance of adequate nutritional support extends beyond basic sustenance. Optimal nutrition facilitates tissue repair and immune function, both vital for the body's ability to recover from radiation's effects. This process allows for faster healing of damaged oral tissues and minimizes the risk of complications. Without proper nutritional support, the recovery process can be prolonged and potentially more challenging. Successful outcomes depend upon a strong understanding of how nutritional interventions can influence healing and minimize adverse effects of radiation treatment. This understanding is crucial for creating personalized dietary strategies that promote patient well-being and successful recovery.
3. Communication
Communication plays a critical role in the recovery process following radiation therapy. Impaired oral function, a common consequence of radiation, can significantly affect communication. Difficulty with speech articulation, swallowing, and the ability to form clear sounds can lead to social isolation and emotional distress. This is particularly relevant when considering the broader context of recovery, which encompasses physical, emotional, and social well-being. Practical examples include the inability to participate fully in social activities, difficulty with interactions with loved ones, and the challenges in conveying needs and feelings. Effective communication during this time is vital to facilitating emotional processing and promoting a sense of connection with others.
The impact of communication difficulties extends beyond immediate interactions. Reduced communication capabilities can hinder effective participation in rehabilitation exercises and discussions with healthcare professionals. This can lead to missed opportunities for support and treatment optimization. Furthermore, communication challenges can influence adherence to medical regimens, as patients might struggle to understand instructions or provide feedback on their progress. For instance, an inability to articulate discomfort or dietary restrictions could lead to complications and hinder the recovery process. Clear and consistent communication between patients, healthcare teams, and support systems is vital for comprehensive patient care. This includes providing appropriate communication aids, such as visual aids, and adapting communication methods to ensure understanding.
In conclusion, effective communication is integral to successful recovery after radiation therapy. The challenges posed by impaired oral function necessitate attentive and flexible communication strategies. Addressing communication needs through personalized approaches, support systems, and accessible tools is critical to the broader rehabilitation process. Overcoming these communication barriers fosters a more positive and supportive environment, ultimately leading to improved patient outcomes and a higher quality of life. The ability to articulate needs, understand treatment plans, and maintain social connections is crucial for the comprehensive healing process.
4. Pain Management
Pain management is a critical component of successful recovery following radiation therapy, particularly in the context of potential long-term oral and swallowing difficulties. Radiation therapy, especially in the head and neck region, can cause significant damage to tissues, leading to various post-treatment pain syndromes. The severity and duration of this pain can differ greatly depending on individual factors and treatment protocols. Effective pain management strategies are essential for restoring oral function, facilitating nutritional intake, and enhancing quality of life.
Pain arising from oral and swallowing complications post-radiation can manifest in diverse ways, impacting patients' ability to eat, drink, and communicate. Inflammation, sores, and altered tissue structure within the mouth and throat create discomfort and, in extreme cases, can lead to debilitating pain. This pain can significantly interfere with a patient's ability to participate in rehabilitation exercises or adhere to dietary restrictions designed to promote healing. Chronic pain can lead to nutritional deficiencies, hindering the recovery process and potentially increasing the risk of complications. Effective pain management is thus crucial for promoting optimal healing, encouraging adherence to treatment plans, and ensuring patients can resume normal activities as quickly as possible. Examples of effective pain management strategies include the use of oral analgesics, topical anesthetics, and in certain cases, stronger pain medications prescribed by physicians. Regular follow-up and adjustments to the pain management strategy are essential, as the severity of pain can fluctuate during recovery.
Understanding the connection between pain management and recovery from radiation therapy underscores the importance of a comprehensive approach to care. Effective pain management is vital not only for physical comfort but also for psychological well-being. Chronic pain can lead to stress, anxiety, and depression. Addressing pain effectively supports patients' emotional resilience and allows them to engage more actively in their rehabilitation. Furthermore, appropriate pain management promotes adherence to post-treatment recommendations, reducing the risk of complications and optimizing recovery outcomes. By prioritizing effective pain management strategies tailored to individual needs, healthcare providers can create a pathway for patients to regain their physical and emotional well-being. This comprehensive approach is crucial to ensuring successful outcomes and a higher quality of life post-treatment.
5. Fatigue Reduction
Fatigue is a significant symptom experienced by many individuals undergoing radiation therapy. This fatigue can stem from the treatment itself, the side effects associated with it, or the overall stress of undergoing such treatment. The impact of this fatigue extends beyond simple tiredness. It can significantly impair a patient's ability to engage in activities of daily living, participate in rehabilitation programs, and adhere to post-treatment recommendations, potentially hindering the recovery process. Effective fatigue reduction strategies are therefore essential to optimize recovery from radiation therapy. Reduced fatigue can directly correlate with better patient outcomes and quality of life.
Addressing fatigue requires a multifaceted approach. Strategies may include but are not limited to physical and occupational therapy to promote strength and endurance. This may also involve strategies for improving sleep quality, managing stress, and optimizing nutritional intake. Appropriate rest and pacing are also critical to counteract the effects of fatigue. Understanding the interplay between fatigue, treatment regimens, and overall health conditions is vital in formulating effective intervention strategies. For example, individuals with concurrent medical conditions or those receiving multiple treatments may experience more pronounced fatigue, requiring tailored approaches to mitigate its impact. Real-life examples highlight how fatigue can limit participation in rehabilitation, hindering progress and potentially prolonging the recovery period. The practical consequence of this is reduced ability to resume normal daily activities.
Fatigue reduction represents a crucial aspect of post-radiation recovery. It's vital to recognize fatigue not simply as a symptom but as a significant factor impacting an individual's ability to participate in rehabilitation and manage their daily lives. Strategies to address fatigue directly contribute to a more positive patient experience, empowering individuals to effectively cope with the treatment process and promote successful recovery. Failure to adequately address fatigue can have long-term effects, impacting patients' overall quality of life beyond the immediate post-treatment period.
6. Quality of Life
Quality of life (QoL) is intrinsically linked to the recovery process following radiation therapy, particularly in the context of oral and swallowing challenges. Radiation therapy, while vital for treating certain conditions, can have significant side effects, impacting various aspects of daily life. The extent of these impacts directly influences the patient's ability to maintain or regain a satisfactory QoL post-treatment. Disruptions to oral function, such as difficulty eating, speaking, and maintaining oral hygiene, can profoundly affect an individual's self-image, social interactions, and emotional well-being. These factors contribute to a reduced QoL.
The connection between QoL and post-radiation recovery extends beyond immediate physical discomfort. Long-term consequences of radiation-induced damage to oral tissues can negatively affect dietary choices, nutritional intake, and overall health. These issues create a cycle: reduced nutrition impacts overall strength and resilience, potentially delaying healing and increasing the risk of further complications. Reduced QoL can manifest as social isolation, limitations in occupational pursuits, and diminished participation in recreational activities. For example, difficulty chewing and swallowing can restrict food choices, impacting nutritional intake and overall health. This, in turn, can affect mood and energy levels, leading to a further decline in QoL. Individuals may become withdrawn from social activities due to embarrassment or difficulty communicating effectively, further diminishing their QoL.
Understanding the profound link between QoL and post-radiation recovery is critical for healthcare providers. Implementing measures to preserve or enhance QoL during and after treatment is essential. This involves proactive management of oral complications, tailored nutritional support, and readily accessible communication strategies. Early intervention and ongoing support, encompassing psychological counseling and speech therapy, become key components in supporting patients through their recovery journey. Ultimately, prioritizing and actively addressing QoL concerns contributes to a more positive and successful outcome, empowering individuals to reclaim their functional independence and sense of well-being after radiation therapy.
7. Psychological Impact
Radiation therapy, particularly for head and neck cancers, can have profound psychological consequences for patients, extending beyond the physical challenges of treatment. This impact necessitates consideration alongside the physical recovery, recognizing that mental health is crucial for successful rehabilitation. The concept of "hisashi ouchi after radiation" implies an extended period of recovery, which underscores the long-term potential for psychological distress.
- Anxiety and Fear
Patients often experience heightened anxiety and fear related to the treatment process. This includes concern about the effectiveness of the treatment, potential side effects, and the impact on future well-being. The prospect of long-term complications, including potential speech or swallowing difficulties, can amplify these anxieties. Fear of recurrence or worsening condition further contributes to distress. In this context, a prolonged recovery period, like "hisashi ouchi," may increase vulnerability to such anxieties.
- Body Image Concerns
Physical changes resulting from radiation, including scarring or changes in appearance, can significantly affect body image. This is particularly relevant in the context of "hisashi ouchi," where patients may grapple with these changes over a more extended period. Difficulty with swallowing and speech can further impact self-perception, leading to feelings of inadequacy, shame, or social isolation.
- Depression and Low Mood
The cumulative effects of treatment, along with the uncertainty surrounding long-term health outcomes, can increase the risk of depression and low mood. The prolonged nature of recovery, as suggested by "hisashi ouchi," can prolong these feelings, requiring proactive support and intervention. Changes in social roles, reduced physical capacity, and perceived limitations further impact psychological well-being.
- Social and Relationship Challenges
The difficulties related to communication and swallowing, often associated with "hisashi ouchi," can lead to social isolation. Patients may feel anxious or embarrassed about their altered appearance or abilities, impacting their social interactions and relationships with loved ones. The strain on personal connections can worsen feelings of isolation and contribute to emotional distress. Family support becomes crucial during this phase of recovery.
The psychological impact of radiation therapy, particularly during the extended recovery period often implied by "hisashi ouchi," is multifaceted and requires careful consideration. Addressing anxiety, body image concerns, depression, and social challenges is integral to overall patient well-being and effective rehabilitation. A holistic approach to care, encompassing both physical and psychological support, is essential to facilitating a smoother and more positive recovery journey.
Frequently Asked Questions
This section addresses common questions and concerns regarding the extended recovery period ("hisashi ouchi") following radiation therapy. Accurate information and understanding are crucial for navigating this process.
Question 1: What does "hisashi ouchi" mean in the context of radiation therapy?
Answer: "Hisashi ouchi," roughly translating to "extended stay" or "long recovery," refers to the prolonged period of healing and rehabilitation that can follow radiation therapy, particularly in the head and neck region. This extends beyond the immediate treatment phase and encompasses addressing the lasting effects on oral health, nutrition, communication, and overall well-being. It is characterized by a gradual and sometimes unpredictable recovery process.
Question 2: What are some common side effects associated with this extended recovery period?
Answer: Common side effects include but are not limited to: oral mucositis (inflammation of the mouth's lining), xerostomia (dry mouth), dysphagia (difficulty swallowing), pain, fatigue, and potential communication challenges. The severity and duration vary considerably depending on the individual and the type and extent of radiation therapy.
Question 3: How can individuals manage the prolonged recovery period after radiation?
Answer: Effective management involves close collaboration with healthcare professionals, including oncologists, dentists, dietitians, and speech therapists. Personalized care plans are essential, addressing specific needs and challenges, and may incorporate techniques for managing pain, promoting oral hygiene, improving nutrition, and facilitating communication.
Question 4: What role does nutrition play in the recovery process?
Answer: Proper nutrition is crucial during "hisashi ouchi." Dietary adjustments, sometimes including soft or liquid diets, may be necessary to alleviate discomfort and ensure adequate nutrient intake. The goal is to maintain energy levels and support tissue repair. Nutritional counseling can provide specific dietary recommendations to support recovery.
Question 5: How long does the "hisashi ouchi" period typically last?
Answer: There's no fixed timeframe for "hisashi ouchi." Recovery is highly individualized. Factors influencing the duration include the type of cancer treated, the dose of radiation, the patient's overall health, and the effectiveness of supportive therapies. Regular follow-up with healthcare providers is crucial to monitor progress and adjust management plans as needed.
A crucial takeaway is the importance of patient-centered care in navigating the "hisashi ouchi" period. Individuals experiencing this extended recovery should seek comprehensive support from their medical team and utilize available resources to enhance their overall well-being. This commitment to multifaceted care plays a significant role in promoting a positive and successful recovery.
This concludes the frequently asked questions section. Further inquiries should be addressed with a healthcare professional.
Conclusion
The extended recovery period, often referred to as "hisashi ouchi" after radiation therapy, represents a multifaceted challenge requiring comprehensive care. This period is characterized by a range of potential complications, including oral health issues, nutritional deficiencies, communication difficulties, pain management concerns, fatigue, and psychological distress. Effective strategies for managing these complications are crucial for optimal recovery. The article emphasized the importance of individualized care plans, incorporating strategies to address oral health, nutrition, communication, pain, fatigue, and the profound psychological impact of the treatment. The intricate interplay of these factors necessitates a holistic approach encompassing medical, dental, nutritional, and psychological support.
The "hisashi ouchi" phase underscores the necessity for proactive and ongoing care. Recognizing the long-term implications for quality of life, effective management of the recovery process is critical. Proactive management, along with tailored support systems, can facilitate a smoother, more positive trajectory for patients. Future research and development should focus on interventions that mitigate long-term side effects and improve the overall patient experience during this extended recovery period. Ultimately, a commitment to comprehensive care and support is paramount for successful and dignified rehabilitation after radiation therapy.
Article Recommendations

ncG1vNJzZmibkafBprjMmqmknaSeu6h6zqueaKWfqMFursCnopqanJp6tMDAq6pooJmorrS0yGamrpuYnnqistOeqWaqkZm2osDIqKVnoKSiuQ%3D%3D